Our bodies are designed to have blood sugar levels in a certain healthy range.
Type 2 diabetes is a condition of high blood glucose, where the body has become inefficient or unable to regulate blood sugar levels in the healthy range.
Type 2 diabetes develops primarily due to insulin resistance (most common); or the pancreas’s inability to produce sufficient insulin (less common, often happens after having diabetes for quite a while).
Understanding Insulin
Insulin is a hormone produced by an organ known as the pancreas. Insulin is the main hormone that helps regulate blood sugar levels.
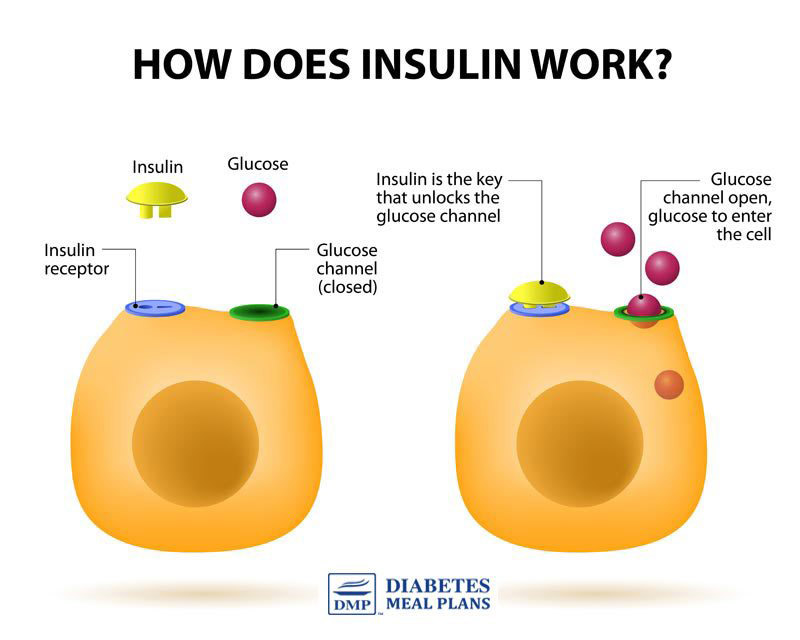
As you can see in the image above, insulin acts like a key that ‘unlocks’ cells to enable the cells to absorb glucose from the bloodstream.
Insulin resistance occurs when the cells in the body don’t respond properly to insulin, so instead of unlocking the cells, glucose (sugar) remains high in the bloodstream.
When your blood sugar levels are high, the pancreas will try to compensate by producing more insulin.
This is quite amazing in one way, as the body has an inbuilt mechanism to try to keep balance in the body with normal blood sugar levels; quite simply because higher-than-normal blood sugar levels is damaging to the bodies cells and vessels, and can even be life-threatening.
The downside is, higher insulin levels increase insulin resistance, which increases blood sugar levels – so the body can get stuck in a vicious cycle.
This is not ideal, as insulin is also a fat storage hormone, so it will push all the excess glucose in your bloodstream to fat, meaning you may put on weight and may struggle to lose it as well.
Your body will be trying to combat the issue of high blood glucose, but the triple whammy of high blood sugar, high insulin, and insulin resistance only makes the issue worse. Eventually, your body loses capacity to efficiently regulate blood sugar levels.
Prediabetes develops
At first you may be diagnosed with prediabetes. Your body is giving signs that it’s on a slippery slope – impaired glucose tolerance, weight gain, high blood pressure and cholesterol are all signs and symptoms.
With prediabetes, you’ve got insulin resistance that is affecting your blood glucose control, but it’s not quite bad enough to be diagnosed with type 2 diabetes.
Type 2 diabetes develops
Eventually, if you don’t do anything about the issue, you will be diagnosed with type 2 diabetes.
Once you have type 2 diabetes, if you still do nothing about the issue, eventually, your pancreas may struggle to produce enough insulin, and you can end up having to use insulin injections.
The great news is that regardless of the stage you’re at, whether you’ve been diagnosed prediabetic, newly diagnosed type 2 diabetes, or you’ve had type 2 diabetes a while – you can reverse insulin resistance and support your body to get back to normal again.
That’s what we teach people to do here at DMP, with our nutrition programs and services.
Risk Factors for Getting Type 2 Diabetes
Several factors contribute to the development of insulin resistance, including genetic, environmental, and lifestyle factors:
1. Genetics
A family history of type 2 diabetes can increase your risk of developing insulin resistance and type 2 diabetes, due to specific gene mutations that may occur. However, while family history may increase your risk, it does not guarantee that you will develop type 2 diabetes, as it’s usually due to a combination of factors.
2. Overweight/obesity
Being overweight or obese is a significant risk factor for insulin resistance.
Excess body fat, particularly around the waist, can fuel low-grade inflammation throughout the body, which can impair the body’s ability to use insulin effectively. Excess body fat also contributes to excess fat in the liver (fatty liver) and excess fat in the pancreas, which make insulin resistance worse.
3. Lack of activity
Let’s face it, we live in technological times, and that brings with it more screen time and less activity.
Lack of physical inactivity contributes to insulin resistance and weight gain, while regular exercise can help improve insulin sensitivity and reduce the risk of type 2 diabetes.
4. Getting older
Sad but true that insulin resistance tends to increase as we get older, particularly after age 45.
This may be due to a combination of factors, such as decreased muscle mass and hormonal changes that affect insulin sensitivity.
5. Ethnicity
Certain ethnic groups have a higher risk of developing insulin resistance and type 2 diabetes, compared to the general population. This includes Aboriginal and Torres Strait Islander peoples, people of South Asian decent, Pacific Islanders, people of Chinese and other East Asian decent, and people from Middle Eastern and North African populations.
6. Poor Quality Nutrition (Most Important!)
One of the primary causes of insulin resistance is poor quality nutrition. Take a look at the picture below – Dr Barry Groves said some wise words!
In general, the modern human diet provides low quality nutrition.
Processed and packaged foods tend to be high in added sugar, low quality vegetable oils, refined ingredients that provide no nutritional value, and a combination of additives and preservatives – many of which have not been tested together so have an unknown effect on the body.
What our body actually needs to function optimally is high quality nutrition.
Quality nutrition is what we teach people to do here at DMP, with our nutrition programs and services.
Practical Action Steps
Some things we can’t change – like our family history, our ethnicity and our age.
The key is to focus on what you can change – the amount of activity you do, losing weight if you need to, and eating a quality diet.
To get started on the right track with a quality nutrition plan, check out:
- Type 2 diabetes foods to avoid – the same principles apply to prediabetes, or even if you just want to lose weight and eat healthier.