Diabetes affects millions of people worldwide; and in Australia there are nearly 1.5 million people living with diabetes.
Type 2 diabetes makes up the largest proportion of people with diabetes in Australia, about 87%; while Type 1 is roughly 9% (yes we know that doesn’t add up to 100%, but that’s the stats according to the NDSS).
Both Type 1 and Type 2 diabetes are characterised by high blood sugar (glucose) levels. However, Type 1 and Type 2 have distinct differences in causes, symptoms, and treatments.
Let’s look closer at the key differences between Type 1 and Type 2 diabetes.
Type 1 Diabetes: Overview and Causes
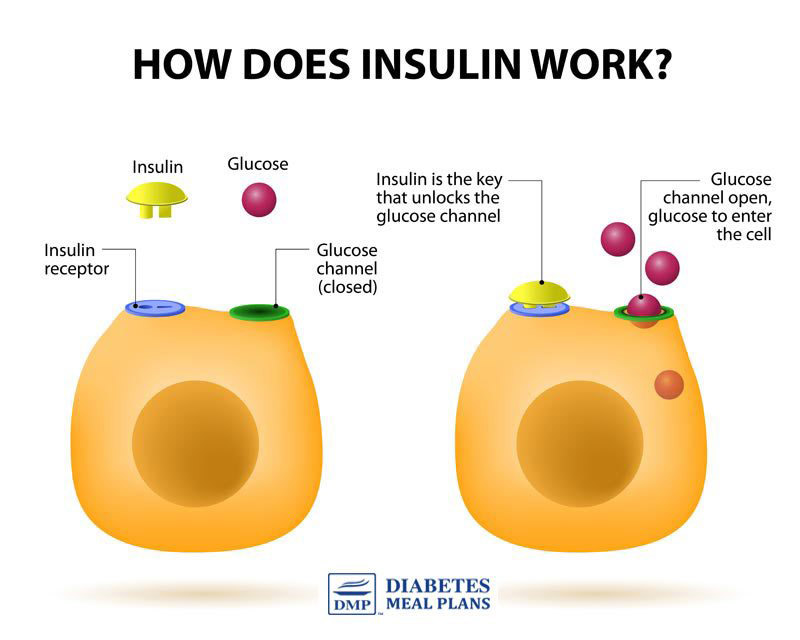
Type 1 diabetes is an autoimmune disease. It occurs when the immune system mistakenly destroys insulin-producing beta cells in the pancreas, resulting in little or no insulin production. Insulin is essential for regulating blood sugar levels, and without it, glucose cannot enter the cells.
Type 1 diabetes is typically diagnosed in childhood or adolescence, and was once also known as juvenile diabetes. However, it is now known that it can develop at any age and some adults can be diagnosed with Type 1.
The exact cause of Type 1 diabetes is unknown; however, a combination of genetic predisposition and environmental factors, such as viral infections, may play a role.
Type 2 Diabetes: Overview and Causes
Type 2 diabetes is primarily a lifestyle-related condition that results from the body’s inability to use insulin effectively (insulin resistance) or due to insufficient insulin production. Majority of people with Type 2 diabetes will have insulin resistance.
As you can see in the picture below, insulin is needed to ‘unlock’ the cells so glucose can enter. With insulin resistance, insulin is unable to ‘unlock’ the cells so glucose can enter, which results in higher glucose levels.
Over time, if nothing is done to control or reverse Type 2 diabetes, the pancreas may become unable to produce enough insulin to maintain normal blood sugar levels.
Type 2 diabetes is more common in adults, particularly those who are overweight, sedentary, and have a family history of the condition. However, it is increasingly being diagnosed in younger people, including children and adolescents, due to rising obesity rates.
Risk Factors
Risk factors for Type 1 diabetes include:
- Family history: A close relative with Type 1 diabetes increases the risk of developing the condition.
- Genetics: Specific genes are associated with a higher risk of Type 1 diabetes.
- Age: Although Type 1 diabetes can occur at any age, it is most commonly diagnosed in children and adolescents.
Risk factors for Type 2 diabetes include:
- Family history: Having a close relative with Type 2 diabetes increases the risk of developing the condition.
- Age: The risk of developing Type 2 diabetes increases with age, especially after 45 years.
- Weight: Being overweight or obese significantly increases the risk of Type 2 diabetes.
- Inactivity: Leading a sedentary lifestyle raises the risk of Type 2 diabetes.
- Ethnicity: Certain ethnic groups, such as Indigenous Australians, are at higher risk.
- Nutrition: Poor quality nutrition is a key risk factor for developing many health conditions, including Type 2 diabetes.
Symptoms
Both Type 1 and Type 2 diabetes share some common symptoms:
- Increased thirst and frequent urination
- Extreme hunger
- Unexplained weight loss
- Fatigue
- Blurred vision
- Slow-healing sores or frequent infections
However, Type 1 diabetes symptoms tend to appear suddenly, while Type 2 diabetes symptoms may develop gradually and be less noticeable.
Treatment and Management
Type 1 Diabetes Treatment
Type 1 diabetes treatment involves lifelong insulin therapy, as the body cannot produce its own insulin.
Insulin is administered through injections or an insulin pump. In addition to insulin, monitoring blood sugar levels, maintaining a healthy diet, and exercising regularly are crucial to managing Type 1 diabetes.
Type 2 Diabetes Treatment
For Type 2 diabetes, treatment typically involves: quality nutrition, losing weight if you need to, and doing regular physical activity.
Oral medications or insulin injections may be necessary if blood sugar levels remain high. However, in many cases, medication can be avoided and even reduced by focusing on quality nutrition. We know because for the past decade, we’ve been supporting people with Type 2 diabetes to treat their condition naturally with nutrition.
Whether you’re newly diagnosed with Type 2 diabetes or you’ve had Type 2 diabetes for 20 years, in many cases you can control or reverse your condition, naturally with nutrition. And even if you need some medication, quality nutrition helps to minimise the amount of medication you may need to take.
Not sure where to start with your nutrition plan? Check out our clinically-proven T2Diet Program.
In as little as 16 weeks, you’ll have your blood sugar and health back on track!