Table of Contents[Hide][Show]
If you’ve heard of fatty liver and diabetes mentioned in conversation, there’s a good reason – they share an intimate connection.
In fact, study after study suggests there are two things that lead to increased development of fatty liver in people with type 2 diabetes – obesity and uncontrolled A1c levels.
Experts estimate anywhere from 6% to 46% of the general population is affected by fatty liver. As a person with type 2 diabetes, the chances of you having a fatty liver are about 80%!
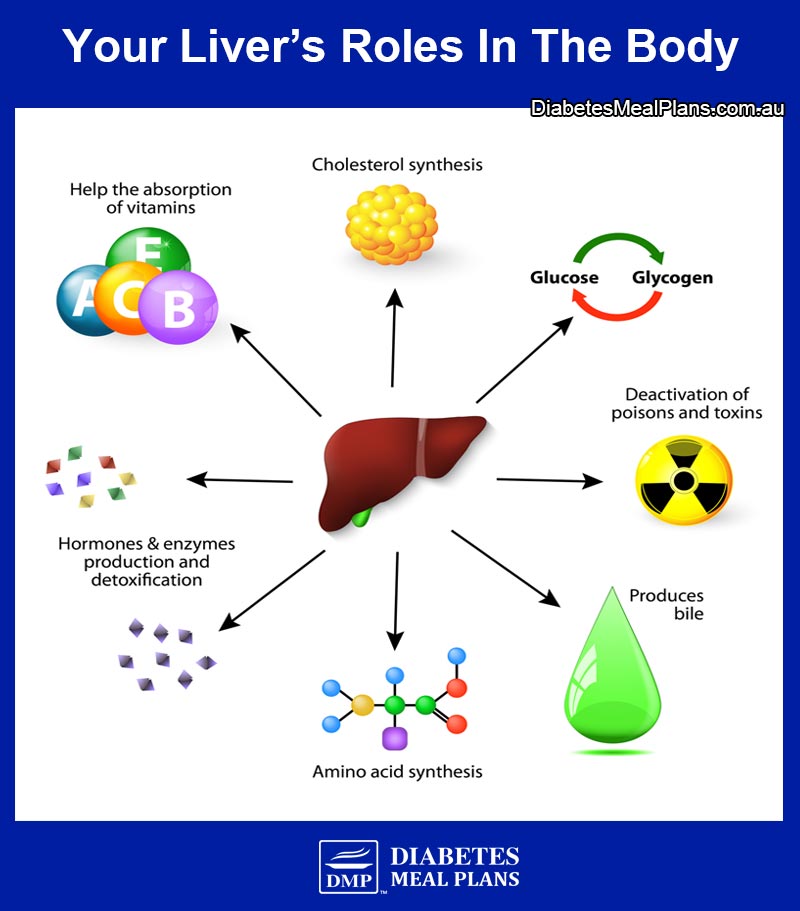
Your liver is the second largest organ in your body. It filters everything you eat and drink, medications you take, and any toxins you may inadvertently consume. And it is intricately involved in metabolic and hormonal balance.
Fatty liver is a concern because it influences how your metabolism is working, including blood sugar regulation. And if left unchecked, a fatty liver can increase your risk of heart disease.
So what exactly is a fatty liver and what can you do about it? Read on to learn more.
What Is A Fatty Liver?
Non Alcoholic Fatty Liver Disease, or NAFLD, is a general term that refers to a build up of fat in your liver. As the name implies, this condition is different from Alcoholic Liver Disease, which is caused by excessive alcohol consumption.
There are two subcategories of NAFLD:
- simple fatty liver – a reversible condition.
- nonalcoholic steatohepatitis, or NASH – the liver cells are inflamed and possibly damaged. This can lead to permanent irreversible liver scarring, also known as cirrhosis, which could potentially lead to liver failure if the damage becomes severe.
People with NAFLD can develop NASH (around 10-25%), although it is not entirely clear why.
Everyone has some fat naturally in their liver. When the weight of fat contained in your liver exceeds 5%, it is considered simple fatty liver. This build up of fat occurs because there is an imbalance between inward and outward flow of fatty acids in the liver. Another way to think of this is that there’s an alteration in the way your body metabolises fats.
What Are The Risk Factors For A Fatty Liver?
General risk factors for NAFLD include:
- Unhealthy diet
- Higher than normal BMI (or in other words, being overweight or obese)
- Hyperlipidemia (high cholesterol levels)
- Type 2 diabetes (or family history of diabetes) – especially uncontrolled diabetes, for instance, having high A1c levels.
Certain medications can also put you at risk of NAFLD, although this is a much less common risk factor compared to the general risk factors described above.
The Connection Between Type 2 Diabetes and Fatty Liver
Due to insulin resistance, people with type 2 diabetes are at a higher risk of developing NAFLD. Changes in hormones such as insulin, along with the presence of insulin resistance, affect enzymes in your body, and this causes an increase in free fatty acids, which can flow into the liver.
Other aspects of metabolism become affected too, such as an increased production of fat formation (called lipogenesis). These factors are promoted by high blood sugar and high insulin levels, which leads to a chain of metabolic events that drive up fat production in the liver. And a cycle can occur where there is an imbalance between inward and outward flow of fatty acids in the liver.
Factors associated with insulin resistance can promote NAFLD, but it also works in reverse, meaning that your fatty liver further promotes insulin resistance. That means doing what you can to reverse and improve liver function, is also very important to your diabetes treatment.
Your diet also plays a key role in the production of excess liver fat.
Your liver cells will convert excess glucose (carbs) into fat. If you’re consuming excess glucose (carbohydrate) and not utilising it for energy, then the excess will be stored as fat. Some of the fat is stored as abdominal (belly) fat, whereas it can also be stored in other cells including your liver.
Fructose in particular has been shown to increase fat deposits in your liver.
Fructose is:
- a naturally occurring sugar found in fruit
- sugar is 50% fructose
- honey is 50% fructose
- agave is 75-85% fructose
- it is also infamously known as the main constituent of high fructose corn syrup
We encourage all people with diabetes and prediabetes to limit their intake of fructose-containing foods.
What Are The Symptoms Of Fatty Liver?
Most people who have a fatty liver experience no symptoms at all. In fact, even if the condition progresses to NASH or cirrhosis there are rarely noticeable symptoms.
Some people (but very few) may notice a discomfort in the right upper quadrant of the abdomen. And jaundice, or yellowing of the eyes and skin, can be a sign of liver cirrhosis.
How Does A Fatty Liver Get Diagnosed?
Since there are relatively few symptoms of NAFLD/ NASH, the diagnosis is often accidental. This means your doctor may bring up concern of NAFLD during routine blood work or an unrelated abdominal imaging study. In some cases a liver biopsy may be warranted as this is the gold standard of diagnosing NAFLD.
Blood Test
One of the first signs of NAFLD is an abnormal liver test identified through blood work. Inflamed liver cells may leak higher-than-normal amounts of transaminase (enzymes) into your bloodstream.
Alanine aminotransferase (ALT) and aspartate aminotransferase (AST) are the two enzymes of particular interest. And while both are elevated in NAFLD, you will classically find that ALT exceeds that of AST.
Imaging Studies
Abdominal ultrasounds and magnetic resonance imaging (MRI) can also aid your doctor in diagnosing NAFLD as fatty liver will show up differently on these scans. Although, imaging studies are unable to differentiate between simple fatty liver disease and NASH.
Liver Biopsy
Your doctor will recommend if he or she feels you need a liver biopsy to diagnosis NAFLD, though, for some people it’s impractical or cost prohibitive to have a biopsy completed.
However, a biopsy can differentiate between NAFLD and NASH. By analysing the tissue itself, your healthcare team can better assess the amount of inflammation in your liver, the amount of permanently damaged cells, and of course rule out any concern for malignancy (cancer).
NAFLD is not caused by heavy alcohol consumption. In order for a true NAFLD diagnosis, a person must report abstinence or very minimal alcohol consumption (<20g/day).
6 Ways to Reverse or Prevent Fatty Liver
The good news about all this, is that there is evidence that fatty liver can be prevented and reversed. That’s why it’s imperative to take action as soon as possible, because once permanent damage occurs it cannot be reversed with any intervention.
#1: Intensive Lifestyle Intervention
Research involving over 5000 participants with type 2 diabetes demonstrated that 12 months of intensive lifestyle intervention can result in up to a 50% decrease in liver fat deposits. The intensive intervention included losing 10% of one’s body weight, and completing 175 minutes of exercise weekly.
175 minutes of exercise per week is equivalent to about 30 minutes a day 6 days per week, which is an achievable goal for most people. But if you’re just getting started even 10 minutes a day is worthwhile – any exercise is better than no exercise at all! And if you are overweight, aiming to lose a few pounds is a great goal to pursue – both exercise and dietary changes can help with that.
#2: Lower Blood Sugar & A1c Through Diet
Controlling blood glucose levels to promote proper glucose utilisation and prevent exacerbation of insulin resistance is another key to success. The best way to achieve better results is to change your diet.
Based on research, and the success of our members, lowering blood sugar and HbA1c is more easily achieved by following a low carbohydrate diet. Check out our free ‘get started’ resources. And we’d highly encourage you to consider our weekly low carb meal planning service – it’s changing lives! Let us help change your life too!
#3: Switch Your Fats
The type of fat (fatty acids) you consume can determine how your body uses them and even where the fat is stored.
Long chain omega-3 fatty acids are classically known for their anti-inflammatory effects and may be useful in the treatment of NAFLD. A 12-month study found that adding 1 gram of omega 3 fatty acid supplementation improved NAFLD.
Another larger study (2008) also found omega-3s of great benefit to a fatty liver.
The researchers divided participants into two groups:
- group A received 2 grams of omega 3 fatty acid supplement
- group B received a placebo
After 24 weeks of supplementation, 20% of group A was downgraded to zero (no fat in the liver present), compared to just 7% in group B.
Good sources of omega 3 fatty acids include:
- salmon
- walnuts
- flax seeds
- chia seeds
- and of course, fish oil
Medium chain triglycerides (MCT) are another type of beneficial fat. MCTs are known to be transported directly into the liver via the hepatic portal vein; this is different to how any other fat is metabolized. Due to this mechanism, they have been shown to increase fat burning in the liver. Coconut oil is one common source of medium chain triglycerides.
#4: Improve Your Gut Health
Interestingly, researchers have shown that people with simple fatty liver have very different gut bacteria compared to those who progress to NASH (the more severe type of fatty liver disease). This means you can manipulate your gut bacteria to help treat your fatty liver. One way to do this is by encouraging the production of Short Chain Fatty Acids (SCFAs).
SCFAs are produced from fermented fibres in the gut, particularly the large intestine. You can increase SCFAs by increasing your intake of prebiotic fibre-rich foods, such as:
- Asparagus
- Jerusalem artichokes
- Chicory
- Green peas
- Leeks
- Onions
- Shallots
- Spring onions
- Dandelion greens
- Fennel bulb
- Beets
- Cashews
- Garlic
- Pistachio nuts
Supplements containing probiotics is another plausible treatment for NAFLD.
A meta-analysis of studies concluded that probiotics significantly improved liver enzymes ALT and AST, as well as an improving total cholesterol and insulin resistance.
#5: Get Adequate Vitamin D
Another nutrient intricately related to your metabolism is vitamin D. This vitamin was initially thought to only assist with calcium regulation and bone health, but it is now well known that vitamin D is a key player in your immune health, gut health, reproductive health, and endocrine (blood sugar/ hormonal) function.
As we spoke about earlier, insulin resistance, or metabolic syndrome, is a main risk factor for fatty liver. Research has consistently shown than supplementing with vitamin D can improve insulin sensitivity, and therefore improve glycemic control (blood sugar regulation).
Furthermore, vitamin D deficiency is commonly associated with NAFLD and studies are beginning to examine the role vitamin D has on NAFLD markers. It has been proposed that vitamin D may play a role in the progression of liver disease. So being that vitamin D deficiency in diabetes is common, it may be wise to discuss your vitamin D status with your doctor and utilise supplementation as needed.
#6: Take Beneficial Supplements
Two final supplements worth noting are milk thistle and apple cider vinegar.
Milk thistle has long been known to have amazing health benefits for the liver, including providing anti-inflammatory and anti-fibrotic properties.
Apple Cider Vinegar (ACV) can aide in blood glucose management by improving insulin sensitivity by as much as 34%. ACV is a natural liver cleanser and helps improve gut bacteria too. Try taking it before meals, it helps lower blood sugar too!
Conclusion
It’s not just your pancreas that’s important to consider in diabetes treatment because your liver is also intricately involved in metabolism and blood sugar regulation. And unfortunately, fatty liver and diabetes often go hand in hand.
The good news is you can prevent or treat fatty liver by making changes to your diet and lifestyle. And adding a few supplements can help too.